 At the Australian Centre for Disease Preparedness, our high-containment biosecurity facility, we are screening antiviral therapeutics to assess the efficacy of their antiviral capabilities against SARS-CoV-2, the virus that causes COVID-19.
At the Australian Centre for Disease Preparedness, our high-containment biosecurity facility, we are screening antiviral therapeutics to assess the efficacy of their antiviral capabilities against SARS-CoV-2, the virus that causes COVID-19.
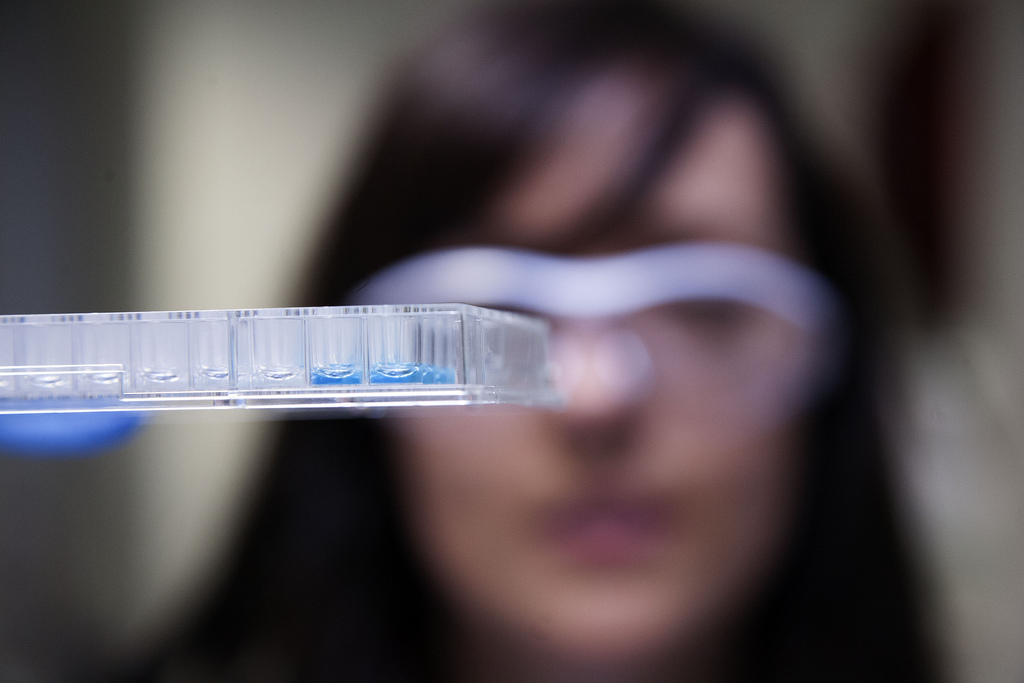
We are conducting three types of screening at our labs: in vitro screening (in cell culture); ex vivo screening (using a model of human epithelial lung cells), and in vivo (animal model) screening.
Using lab-grown ‘lungs’ against respiratory viruses
Our scientists have found that lab-grown human airway cells can reliably be used to study respiratory viruses such as COVID-19, and potentially to fast-track treatments for human trials.
What the study involved
In a study at our Australian Centre for Disease Preparedness, we found that lab-grown cells from the upper layer of the airway to the lungs – the human bronchial epithelium – reliably mimic a live person's airway's response to viruses.
The study involved growing donated human airway epithelial cells on porous membranes exposed to air. When these cultures were infected with the 2009 pandemic H1N1 influenza virus, the cells had the same innate immune response as in a live person’s airway, with the production of cytokines and chemokines.
The results were published in the journal Viruses on 24 June 2020.
Using the model to understand viruses and screen antivirals
This ex vivo model is being used to help study the characteristics of COVID-19 and how it affects airway cells, helping reduce the need for animal testing.
It is being used to ‘fast-fail’ antiviral treatments, by testing whether the treatments work well enough to progress to clinical trials.
At the Australian Centre for Disease Preparedness, our high-containment biosecurity facility, we are screening antiviral therapeutics to assess the efficacy of their antiviral capabilities against SARS-CoV-2, the virus that causes COVID-19.
We are conducting three types of screening at our labs: in vitro screening (in cell culture); ex vivo screening (using a model of human epithelial lung cells), and in vivo (animal model) screening.
Using lab-grown ‘lungs’ against respiratory viruses
Our scientists have found that lab-grown human airway cells can reliably be used to study respiratory viruses such as COVID-19, and potentially to fast-track treatments for human trials.
What the study involved
In a study at our Australian Centre for Disease Preparedness, we found that lab-grown cells from the upper layer of the airway to the lungs – the human bronchial epithelium – reliably mimic a live person's airway's response to viruses.
The study involved growing donated human airway epithelial cells on porous membranes exposed to air. When these cultures were infected with the 2009 pandemic H1N1 influenza virus, the cells had the same innate immune response as in a live person’s airway, with the production of cytokines and chemokines.
The results were published in the journal Viruses on 24 June 2020.
Using the model to understand viruses and screen antivirals
This ex vivo model is being used to help study the characteristics of COVID-19 and how it affects airway cells, helping reduce the need for animal testing.
It is being used to ‘fast-fail’ antiviral treatments, by testing whether the treatments work well enough to progress to clinical trials.
